Localization can be an Answer to the Double Burden of HIV and Gender-Based Violence
By Shubh Swain, WI-HER Senior Associate
Sarah, a young woman living with HIV in Eastern Uganda, depended on regular antiretroviral therapy (ART)[1]to stabilize her health. Shortly after Sarah’s mother moved Sarah and her family into her partner’s home, Sarah and her mother began to experience repeated domestic violence. As the violence intensified, Sarah fled and started missing her ART and health check-ups. The violence not only endangered Sarah’s life but also put her partner’s health at risk due to Sarah’s HIV-positive status. Unfortunately, Sarah’s story is not an uncommon one, as many young women and girls struggle with the double burden of HIV and gender-based violence (GBV), including in Africa.
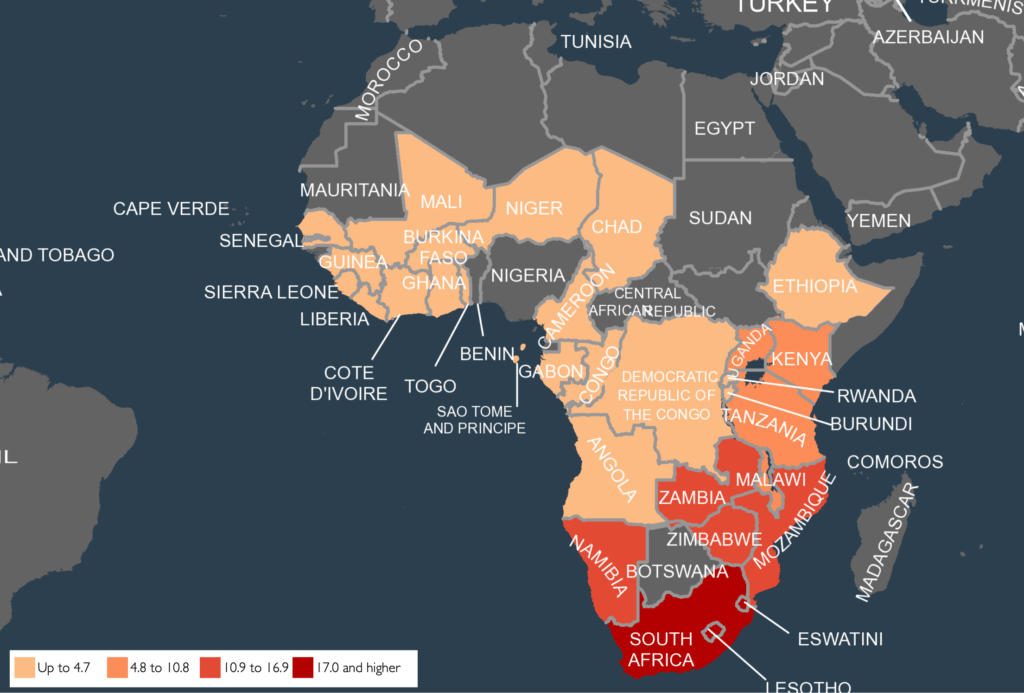
African countries have made significant strides in controlling and minimizing HIV prevalence over the last three decades. The number of people who acquired HIV among all ages decreased to 0.57 [0.41–0.8] per 1000 uninfected population in 2022 from 1.75 [1.24–2.44] in 2010. Despite these successes, HIV/AIDS remains one of the top-ranking public health threats in the continent, where 17.8% of the global population lives. Moreover, the continent is home to 69% of the people living with HIV worldwide.
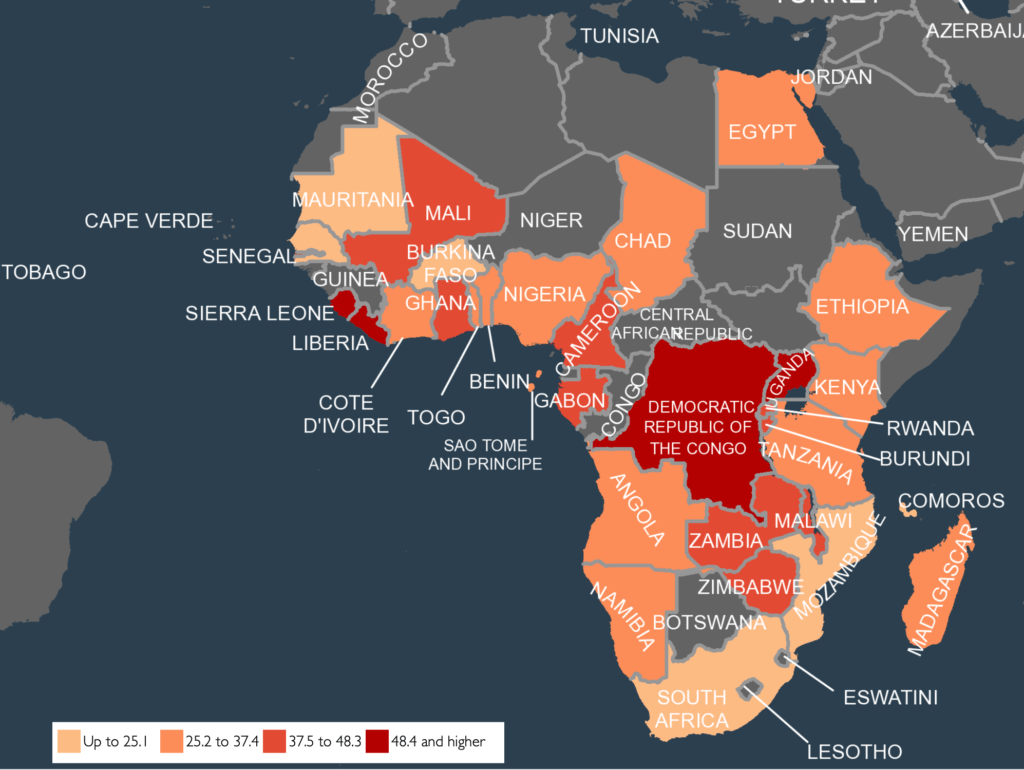
In addition to HIV, GBV is also a prevalent public health and human rights concern. UN Women reports that, globally, one in every three women has experienced either physical or sexual violence in their lifetime. The report estimates that in some African countries, the percentage of women who have experienced violence is as high as 71%.
The vulnerability circle of HIV and GBV
The complex relationship between HIV and GBV is multi-dimensional because, for instance, GBV can increase the risk of new HIV infection. As the data shows in a multicounty large cohort study, women who have experienced intimate partner violence (IPV) have an adjusted incidence rate ratio (IRR) of incident HIV infection of 1.55 (95% CI 1.25-1.94, P = 0.000), compared to women who had never experienced IPV.
The relationship between HIV and GBV is also influenced by the fact that GBV can contribute to restricted access to HIV prevention, care, and treatment. Multiple sources (Cabral, A. et al., 2018; Cluver, L. et al., 2018; Merrill, K.G et al., 2020; WHO, 2013) state:
1) GBV is a barrier to pre-exposure prophylaxis (PrEP) initiation and adherence;
2) Women who experience IPV may be less likely to access HIV testing services or disclose a positive HIV diagnosis due to fear of violence; and,
3) Violence, particularly IPV, can result in lower CD4 counts[2], higher viral loads, and lower adherence to treatment for women and girls.
The increased HIV risk can also be a reason for GBV. HIV-infected or affected women and girls have a higher risk of stigma, denial of treatment, refusal of resources, exclusion from social and familial safety nets, forced reproductive behavior, physical violence, and femicide (UNAIDs, 2017; Valverde et all 2018; Li et all , 2019). This cause-and-consequence relationship feeds into the vulnerability cycle of HIV and GBV.
In recognition of the relationship between GBV and HIV, governments, international development agencies, and civil societies are collaborating on programs that aim to break the link between HIV and GBV. Still, we must do more to break the vulnerability cycle of HIV and GBV by piloting and scaling innovative methods for sustainable and faster results.
One such innovative method is WI-HER’s iDARE™ methodology, as it can be used to identify multi-dimensional, context-specific factors related to GBV and HIV and ensure that local stakeholders understand those factors when designing solutions that make the most sense for them, no matter their community or country.
WI-HER’s iDARE methodology demonstrates a path forward
WI-HER, a leading collaborator on many global efforts to address health and human development issues across Africa, has built the capacity of local stakeholders to use iDARE™ to find solutions related to HIV and GBV. Based on the science of improvement and focused on the continuous identification and documentation of barriers, the iDARE methodology evolved through years-long operationalization and learning through programmatic interventions into an iterative five-step process that can be implemented in any context to address any development challenge.
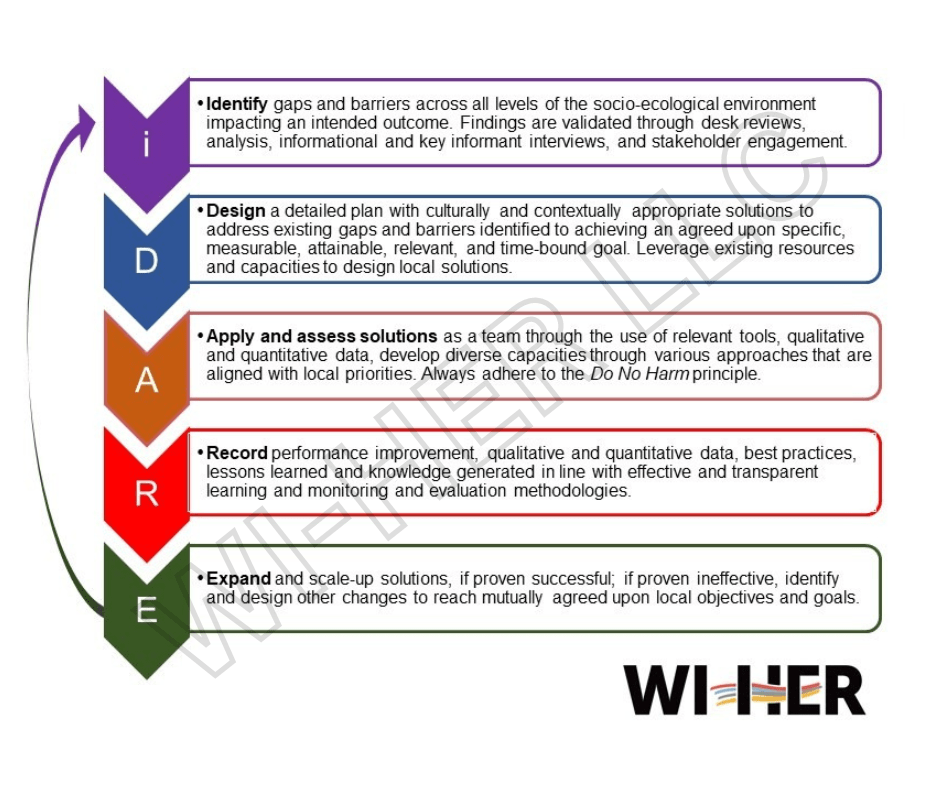
Practitioners who piloted iDARE across countries and disciplines recognized that, for most issues, the solution must be local. Since the methodology’s inception, iDARE has been an effective tool for understanding local barriers to desired outcomes, designing solutions with local resources, applying the solution through local agencies, and generating evidence for scaling up.
In many WI-HER-led programs, managers, local implementers, and community stakeholders use iDARE to make health and other services more gender and social-inclusive.
Enhancing HIV and other health services through behavior change: In Uganda, within the USAID-funded Social and Behavior Change Activity (SBCA), the WI-HER team—in partnership with prime John Hopkins Center for Communication Programs—engaged local community leaders to apply iDARE to identify the gaps restricting inclusive access to services like antenatal care, tuberculosis, immunization, family planning, and HIV/AIDS care. Through the use of iDARE, the program not only witnessed an increase in health services related to vaccination and TB but also witnessed improvements in HIV/AIDS care and declines in HIV-related stigma while also seeing the enhanced capacity of health service providers.
Reducing HIV risk among vulnerable populations through gender and social inclusion: The USAID-funded Adolescents and Children, HIV Incidence-reduction, Empowerment, and Virus Elimination (ACHIEVE) project aimed to make HIV/AIDS service and care more gender sensitive. In Rwanda, ACHIEVE aimed to control and sustain the HIV/AIDS epidemic among the most at-risk and hard-to-reach pregnant and breastfeeding women, infants, children, and adolescents. The PEPFAR-funded program not only ensured a safe space for vulnerable adolescent girls and young women to seek services, but it also created a line of sensitized and well-equipped caregivers at the family and facility levels. With the use of iDARE, the program reported increased viral load suppression among target groups within a short period (60% to 100% among boys and 85% to 100% among all adolescents in the intervention district).
In Tanzania, the program focused on orphans, vulnerable children, and at-risk adolescent girls and young women to improve their access to HIV-inclusive services. Utilizing iDARE, the team from WI-HER and prime implementing partner PACT identified gaps through an analysis and laid out solutions toward more HIV-inclusive social services. The iDARE methodology-driven interventions enabled social welfare providers to deliver more gender-inclusive care and enriched a training guide for integrating GESI.
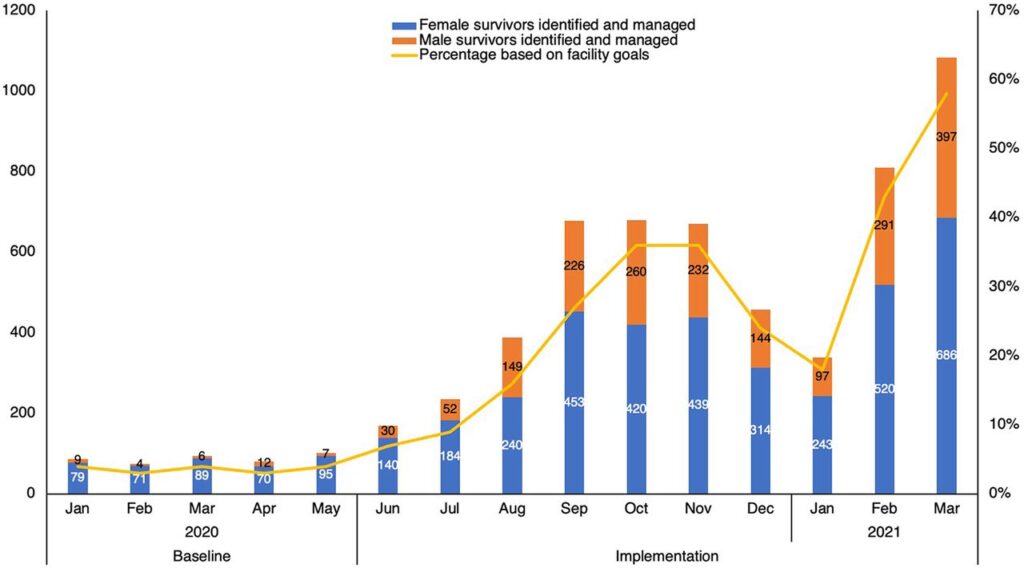
Improving GBV identification and responses in healthcare facilities: In Kenya, WI-HER was a lead partner focused on improving GBV response in the health system in the USAID-funded Afya Nyota ya Bonde project led by prime FHI-360. Before the program was initiated, data showed that almost half of the women and girls in Kenya had experienced GBV. However, the service access rate was as low as 8% among GBV survivors.
Through the implementation of iDARE, the WI-HER team, along with FHI-360 and the Kenya government GBV focal person in the health facility, identified structural and cultural barriers to service access and co-designed solutions that involved sensitizing the management and other departments to include GBV screening and referrals, multiple trainings to capacitate the service providers for better identification of GBV, and community-level sensitization on health services. The multifaceted approach resulted in improved GBV identification and referrals within 12 months (see Figure 4).
WI-HER’s iDARE methodology fosters an understanding of the barriers at the lowest level possible, designing and applying solutions by involving local stakeholders who are better familiar with the local context and own the process across countries, cultures, and sectors, especially when the issues are complex and rooted in regional dynamics. While dealing with the chronic entwined intersections of GBV and HIV, WI-HER’s iDARE methodology can be a powerful tool to mitigate this double burden.
[1] Antiretroviral therapy (ART) is treatment for people infected with human immunodeficiency virus (HIV) using anti-HIV drugs that suppress HIV replication.
[2] A CD4 count is a blood test that measures the number of CD4 cells in a sample of a person’s blood. CD4 cells are a type of white blood cell that triggers the immune system. In a HIV infected person a low CD4 count means that HIV has weakened the immune system. A CD4 count of 200 or fewer cells per cubic millimeter means that you have AIDS.