The Potential of m/eHealth to Improve Newborn Health, a Gender Perspective
By Elizabeth Romanoff Silva, MPA on February 23, 2014
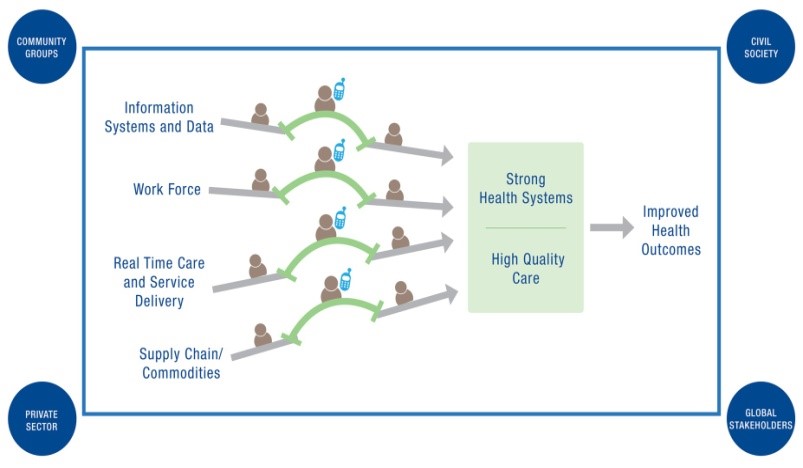
“Every system is perfectly designed to achieve exactly the results it achieves.” USAID Applying Science to Strengthen and Improve Systems (ASSIST) Deputy Director Kathleen Hill shared this quote from Deming with an audience of more than 40 leading experts in technology, health care, and international development that gathered on January 31st in Washington, D.C. for an m/eHealth Health System Strengthening technical working group meeting. The Bridging the Gaps: Leveraging m/eHealth to Achieve Strong Health Systems and High Quality Care in Low-Resource Settings technical meeting considered a working framework developed by the USAID ASSIST project and discussed how m/eHealth solutions can bridge common quality and systems gaps in low-resource settings to augment system strengthening and quality improvement efforts to achieve better health outcomes.
As a gender specialist working for WI-HER LLC on the ASSIST project, my interest in m/eHealth is twofold: first, I am examining how technology can be leveraged to transform traditional gender norms to improve health outcomes for women, men, girls and boys. My second interest is in mitigating the negative impact that m/eHealth interventions can potentially have on gender relations. One of the biggest takeaways from the meeting for me was the idea that technology is often developed and packaged as a solution before the problem and its root cause are defined. There can be a lack of discussion and consensus about what the problem is, what response is required to solve the problem and close the gap, and to what extent m/e technology can aid in that. It’s important that the technology solutions benefit the women, men, newborns and children they are meant to serve.
An example of this is the push in recent years to target women through mHealth interventions, sometimes without sufficiently analyzing whether the problem warrants a response which includes an mHealth solution focused on women exclusively. If the problem identified, for example, is that neonatal mortality is very high, and it is observed that very few mothers in the community receive antenatal care (ANC) or deliver with skilled providers, an mHealth project might provide mobile phones to pregnant women and girls and send targeted SMS messages to tell them about the importance of ANC, to remind them to schedule ANC appointments and to deliver with a skilled provider. The reasoning behind this makes sense: mothers who do not receive high-quality ANC and childbirth care are more likely, along with their newborns, to suffer serious consequences of childbirth complications such as pre-eclampsia. But if one of the root causes of pregnant women not attending ANC visits is because the power and decision-making dynamics in households limit women’s and girls’ ability to make health-related decisions, and male partners do not appreciate the value and therefore do not want their partners to attend ANC visits, then the mHealth intervention would not be as effective as it could be. In some cases the receipt of text instruction that challenges the male’s authority in the home, may even put the female at risk. A more appropriate solution which utilizes mHealth would be to design an intervention which, in addition to reaching out to pregnant women, sends messages to male partners about the importance of ANC and appointment reminders for their partners after they have had participated in education and counseling sessions with female partners. This gender-sensitive mHealth intervention would be more likely to lead to increased use of ANC services and skilled delivery care by pregnant women and hence to contribute to improved outcomes for mothers and newborns if the quality of care is high.
The “Bridging the Gaps” meeting highlighted the importance of leveraging m/eHealth solutions as part of broader health system strengthening and QI efforts to achieve better health outcomes for women, men, newborns and children. Specifically, experts in the field discussed strategies for leveraging m/eHealth to strengthen essential health system functions related to service delivery and real time care, workforce, commodities and supply chain, and data and information systems in low-resource settings and identified many areas for participant collaboration. The meeting offered a very useful platform for collaboration and learning and the expectation is that m/eHealth HSS/QI technical working meetings such as this will continue in the future.
The Bridging the Gaps: Leveraging m/eHealth to Achieve Strong Health Systems and High Quality Care in Low-Resource Settings technical meeting was jointly organized by the USAID Applying Science to Strengthen and Improve Systems (ASSIST) Project managed by University Research Co., LLC (URC) with support from the U.S. Agency for International Development (USAID) Office of Health Systems. For more information about USAID ASSIST’s work to leverage technology to improve systems, please contact Allison Foster at afoster@urc-chs.com.