8 Reasons Why – Barriers to Care and Treatment in the Caribbean: What We’ve Learned since the Zika Outbreak
By Morgan Mickle, Gender Specialist, WI-HER, LLC
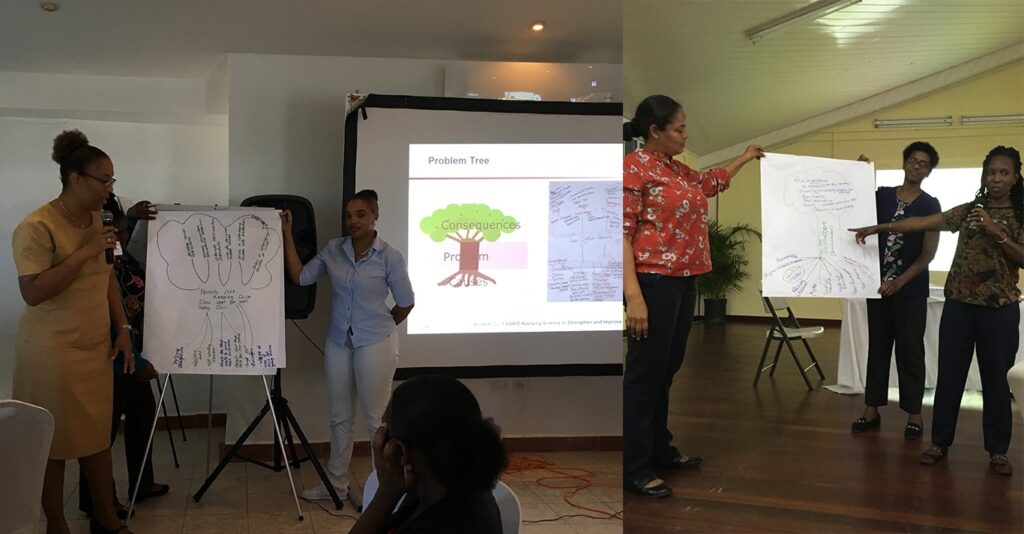
In November and December 2018, I had the privilege to take part in a series of learning sessions across the Eastern and Southern Caribbean – specifically, Antigua, Dominica, St. Kitts and Nevis, and St. Vincent and the Grenadines. As expert gender partner on the USAID ASSIST Project, WI-HER works closely with University Research Co. LLC and its other partner organizations to improve the quality of health care for children, women and families. My participation in the sessions helped emphasize our belief that gender, and social inclusion issues can and should be integrated into existing services. While working in a setting where the turquoise waters and warm air were a welcomed change from the ensuing U.S. winter, my ASSIST and American Academy of Pediatrics (AAP) colleagues and I focused on our mission: to strengthen the capacity of 180 health and education professionals working to advance care of newborns and young infants, child development, and improved health outcomes.
What we learned when applying a gender lens to examine barriers to care and treatment, could shift the face of Zika response.
In all the countries we visited, the topic of “defaulters” from follow up care in general and in the context of Zika in particular, came up. Defaulters, as I learned, refers to patients who do not show up to health facilities when they are supposed to. Okay, so maybe they forgot once, twice, three times…but as a pattern starts to emerge we must take a deeper look and ask ourselves , “What is the reason? What is the bigger picture?” In the context of the Zika response, these questions are particularly important. Antenatal visits enable monitoring of mother and baby and creates a greater chance of early detection of the virus. After a baby is born, standard assessments during routine well-baby visits and are still critical; even for seemingly healthy children. Parents who don’t regularly attend well-baby clinics may miss early opportunities to identify developmental delays, including those at risk of Zika, and start life-changing therapies.
According to the CDC 12, Zika virus infection during pregnancy can lead to a spectrum of health conditions, referred to as congenital Zika syndrome (CZS), that affect development of the unborn child. These health conditions include, smaller than expected head size (microcephaly), problems with brain development, feeding issues, vision challenges, hearing loss, seizures,
problems with joint movement, hypertonia (where too much muscle tone causes stiff movement) and others. These conditions may not be evident at the time of birth but can manifest several years after the child is born and develop at a later stage. While not every woman who is infected with Zika during pregnancy will have a baby with health challenges 3, children who are affected may have needs that require long-term or extensive care.
Some conditions linked with Zika can lead to progress lags in moving, learning, speaking, or playing, and are referred to as “developmental delays.” Early detection can give that child and family a head-start to meet with specialists, receive therapies, and access services that could make a difference in the child’s quality of life. While no active cases of Zika have been reported in these four countries in 2018, there is likely a cohort of children who were exposed to Zika infection while their mother was pregnant and during the peak of the Zika epidemic in these countries (2016-2017), but whose CZS and relevant needs may not have yet been identified. This is where the importance of well-baby visits come in.
Routine well-baby visits – or “clinics” as they are often referred to in the Caribbean – help facilitate early detection of delays and abnormalities through exams that monitor baby’s growth and development. They also provide routine immunizations for children and counseling support for parents and caregivers. The USAID ASSIST project is building the capacity of newborn and well-baby care providers to evaluate infants with possible congenital Zika syndrome, monitor child development, and provide early childhood stimulation using USAID ’s Therapeutic Early Stimulation Toolkit.
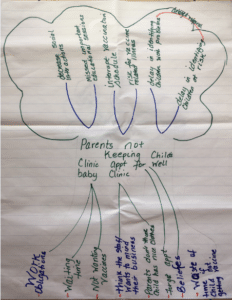 The learning sessions revealed underlying gender issues and challenges affecting uptake in well-baby care. We learned from nurses, doctors, registered midwives, community health aides, and early childhood development specialists, that more mothers than fathers bring their children to well-baby clinics, but a common challenge facing some countries is that parents do not bring their children to well-baby clinics as scheduled. In fact, it is common (as participants in St. Kitts shared) that children miss their well-baby clinics over prolonged periods of time. Defaulting is a complex issue but understanding some of the primary drivers explained below and examining the differing roles, responsibilities, perceptions, attitudes, and behaviors of men, women, and individuals can help decision-makers and health practitioners better reach and sustain health goals.
The learning sessions revealed underlying gender issues and challenges affecting uptake in well-baby care. We learned from nurses, doctors, registered midwives, community health aides, and early childhood development specialists, that more mothers than fathers bring their children to well-baby clinics, but a common challenge facing some countries is that parents do not bring their children to well-baby clinics as scheduled. In fact, it is common (as participants in St. Kitts shared) that children miss their well-baby clinics over prolonged periods of time. Defaulting is a complex issue but understanding some of the primary drivers explained below and examining the differing roles, responsibilities, perceptions, attitudes, and behaviors of men, women, and individuals can help decision-makers and health practitioners better reach and sustain health goals.
8 Reasons Parents and Caregivers Default on Well-baby Clinics :
- Mother’s work obligations and other conflicting interests –mothers often have many obligations in and out of the home and cannot bring their children to clinic. For example, responsibilities in the home may include, washing, cooking, and taking care of other children. Apart from this, mothers may also have competing priorities that take away their time. In Dominica, sometimes it’s just poor planning of daily activities, like wanting to go to the hair salon, that conflicts with the need to do chores. In St. Vincent and the Grenadines, some mothers don’t want to spend “quality” time in the clinic. Well-baby visits don’t always fit in with what activities have been planned for that day or the next.
- Fathers and their perceived roles – while there are instances of fathers bringing children into facilities in all the islands, more often it is the mother who accompanies the child for check- ups. In St. Vincent and the Grenadines for example, fathers are reportedly not willing to bring children to clinic in the mother’s absence. In Dominica, some women have shared with providers that they lack support from their partners in other child health visits as well such as antenatal appointments.
- Fear of stigma and discrimination – some parents and caregivers may feel they will be treated poorly at the health facility by other patients or by health staff. One health worker in Antigua shared that one patient asked if she could bring her child with disabilities through the back door of the health facility because she didn’t want other people waiting in the facility to laugh and mock them. Parents may also be unwilling to bring their children to the clinics because they fear they will be discriminated against for not having “nice enough” clothing. In St. Kitts, if the parent is a teen, they might feel shame for having a child at their age or be hesitant returning to a facility after previously being judged for asking for contraception. Similar fear of reprimand also impacts women who have missed their antenatal screenings.
- Lack of confidence in health providers – past experiences can impact the decision to return to a health facility. In Antigua, patients have said that staff are too intrusive of their lives. If there is bad personal history with a health worker in a small community, a patient may go out of their way to avoid them. Health providers also shared that patients may perceive them to be unskillful at their job if they are unable to perform specific tasks due to a lack of training opportunities beyond their basic, routine functions ; they cited more training opportunities as a way to boost skills and confidence to provide high quality care.
- Lack of education of caregivers – some individuals may not know why well-baby clinics are important and may even portray a “don’t care” attitude. Some parents also think that going to a health facility is a waste of time if their child isn’t receiving a vaccine at that visit.
- Geographic accessibility – clinic locations can be far and inaccessible for some families. Fathers have complained that distance to reach the facility is a deterrent. Utilizing specialized services like referral specialists and unique therapies can be challenging. For populations living in the Grenadines specifically, many specialized services are only offered on the island of St. Vincent and travel back and forth can be a costly expense for patients.
- Overcrowded clinics – in Antigua, boundary changes and population increase coupled with staff shortages and disorganization of shared spaces have left clinics overfull. Staff may not have enough time to assess babies and wait times are often long, frustrating families.
- Religious and personal beliefs – finally, some community members prefer not to go to health facilities because of religious beliefs or customs. The Rastafarian community for example, doesn’t believe in vaccines and the children are therefore exempt from receiving them if the parents opt out.
As a single parent I never used to like going to the health center with my k ids. It was very time consuming and I thought the nurse was fast, asking too many questions … until I became a nurse. I now fully understand and was able to explain to a parent the reason for not missing appointments and the importance of following the child from 0 to 5 with immunizations Nurse working in health clinic, St. Kitts and Nevis
Spotlight – Ideas from the Islands:
- To improve attendance and mitigate instances of default, health facilities must work to increase the awareness among staff to existing barriers to service utilization and act together to tackle them. For example, extending or shifting operating hours would allow more clients to access services at a time convenient to them.
- There must also be outreach efforts to help educate community members about the importance of well-baby clinics and why they are necessary for families. For example, educating all parents about the importance of immunizations, or reaching fathers on the benefits of participating in antenatal sessions and child care.
The implications of missed visits are many – children and families risk an interrupted vaccination schedule, exposure to related illnesses, and possibly contribute to reemergence of diseases in their communities; parents don’t receive important educational information; babies’ social interactions can suffer; and there can be delays in identifying children with developmental challenges (which may further delay a referral) and responding to their needs. In the context of Zika this is especially relevant.
This is why our work to engage more mothers, fathers, caregivers, and family members in well- baby clinics in these settings is so important. A parent or caregiver of a new baby or young child with health conditions related to Zika may feel overwhelmed, worried, and uncertain about the future of their family. For health care workers and providers, it is critically important to identify the different needs of individual family members, adjust the approach to carry-out health services based on those observed needs and constraints, and scale-up what methods work to reach clients. Improvement in care can only be possible through deep understanding of the root causes of problems and testing, implementing, and regularly monitoring the changes to address the identified gap. If clinics can follow this approach, they will be more prepared and more resilient to respond and adapt to any future emerging health priorities. As we continue to respond to the aftermath of Zika in the region, we must reflect on this learning, develop community-specific and locally-acceptable roadmaps, and work through solutions that improve health outcomes and quality of life for all.
From 2012-2017, the USAID ASSIST (Applying Science to Strengthen and Improve Systems) Project fostered improvements in 38 countries in a range of health care processes through the application of modern improvement methods by host -country providers and managers and build the capacity of host – country systems to improve effectiveness, efficiency, client – centeredness, safety, accessibility, and equity of the health services they provide. In a two-year extension from 2017-2019, ASSIST applies quality improvement methods to health systems strengthening efforts in Zika-affected countries, including
Antigua and Barbuda, Dominica, Dominican Republic, Ecuador, El Salvador, Guatemala, Honduras, Jamaica, Nicaragua, Paraguay, Peru, St. Kitts and Nevis, and St. Vincent and the Grenadines.
WI-HER, LLC (Women Influencing Health, Education and Rule of Law) is a woman-owned small business that partners with international donors, national governments, non-governmental organizations and others to identify and implement creative solutions to complex development challenges to achieve better, healthier lives for women, men, girls, and boys. Founded by Dr. Taroub Harb Faramand in 2011, WI-HER, LLC work s to integrate gender through contextualized, adaptable, and systems strengthening methods that can be seamlessly integrated into ongoing and new programs. WI -HER is committed to ensuring equal opportunities for women, men, girls, and boys, as well as all other vulnerable groups, including LGBTQI+ people.