Family Planning as a Shared Responsibility: Improving Reproductive Health Seeking Practices Through Male Engagement in Nigeria
By Adamu Florence Danladi, WI-HER Gender, Social Inclusion, & Community Engagement Advisor
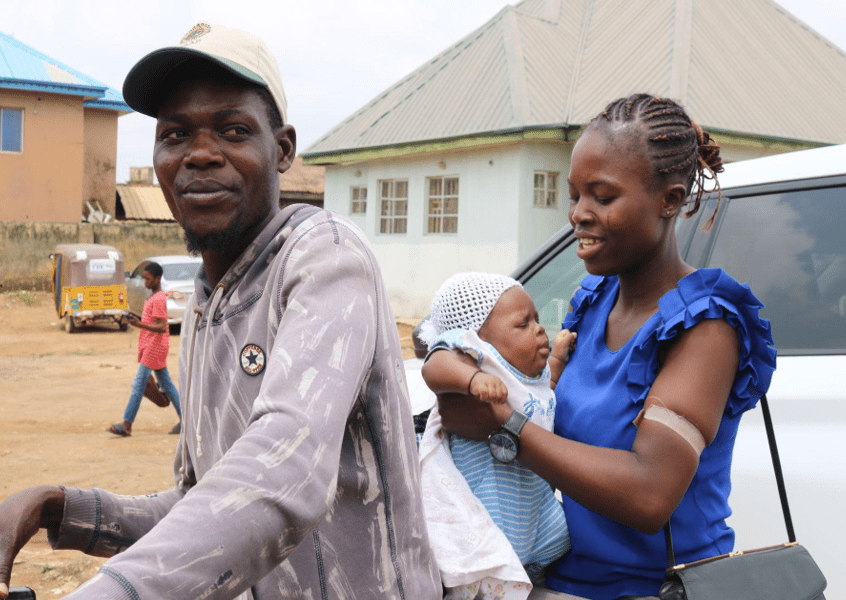
24-year-old Martha[1] is a mother of three children—currently ages two years, 13 months, and 13 weeks. Close birth spacing can often lead to maternal and child health risks such as low birth weight and early child death, and according to research, birth intervals tend to be closer together in rural areas, such as where Martha and her family live in the Federal Capital Territory (FCT) of Nigeria.
When Martha took her three children to a local primary health care facility for their routine immunizations for the first time, she received health education about healthy birth spacing and family planning options available at the health facility. But what made these health education sessions particularly impactful to Martha and other mothers like her is that they encouraged men to become engaged and involved, and Martha returned home and asked her husband to accompany her to the next health education session.
As traditional heads of household in Nigeria, men play a vital role in influencing their families’ health-seeking practices, including the uptake of family planning services. Recognizing the role of men in health seeking, including in the area of maternal and child health, the Government of Nigeria, in collaboration with the USAID Integrated Health Program (IHP), WI-HER, and key stakeholders, such as the Federal Ministry of Health and States Ministries of Health, embarked on a transformative journey to both challenge deeply ingrained socio-cultural norms related to family planning and promote male health-seeking behavior.
Why Addressing Norms, Myths, and Misconceptions Around Family Planning is So Important
In 2022, Nigeria initiated a comprehensive family planning program to address cultural norms—such as the desire for large families, tightly held religious beliefs, and women’s lack of decision-making power—in sexual and reproductive health matters. This initiative aimed to improve the availability and accessibility of family planning (FP) services and commodities, which allows women and their partners to make informed reproductive decisions, thus paving the way for a healthier future for all.
At the core of this effort was dispelling myths and misconceptions surrounding family planning, including, for example, seeing FP as un-Godly and believing it causes cancer and increases the risks of other illnesses. By addressing these myths and misconceptions through health education sessions, the initiative aimed to increase access to healthy family planning.
The program addressed cultural norms, myths, and misconceptions by supporting healthcare workers in 160 health facilities across 62 wards and training at least three skilled healthcare providers per ward on FP services. The trainings included how to provide counseling for all FP services so that clients could make informed choices about their health. Some of this support also involved IHP, in collaboration with Breakthrough Action Nigeria (BA-N) and WI-HER, sensitizing individuals on the importance of FP and what services are available to them.
How USAID IHP Fostered Male Engagement & Expanded FP Services
Through IHP, WI-HER identified the importance of engaging and retaining the support of men to promote health-seeking behaviors. WI-HER’s GESI Advisor and the Gender Unit of the Primary Health Care Board (PHCB) in the FCT then jointly conducted a desk review, which included asking men why they were reluctant to utilize services available in the health facilities. Men shared that they were not being tended to in a timely fashion for their own appointments and that they were not allowed with their partners during antenatal care (ANC) visits and delivery. They felt locked out of the healthcare process throughout their partners’ pregnancy, all the way up to delivery and even post-delivery care.
Based on the findings from the desk review, WI-HER’s GESI Advisor led a series of meetings with PHCB Unit Heads to design activities that fostered the support, allyship, and participation of men beyond just financing healthcare. The health strategies and interventions they designed also addressed men’s unique health needs while also enabling men to make informed health decisions for themselves as well as collaborative decisions with their partners and families. Further, two pilot facilities tested the newly designed activities to see if male engagement participation and retention went up when: 1) men were allowed to accompany their partners in the delivery rooms when it was time to give birth, 2) the health care worker allowed men to sit in for some but not all of the discussions when women visited the health facilities for services, and 3) health facilities created special seating areas for men to wait for their partners when they received services like blood pressure and glucose checks.
Much of this support also involved expanding FP services to the most remote areas of FCT, where there is often low uptake of FP services, including adolescent-friendly services. Community engagement initiatives, similar to the male engagement activities, helped ensure that women, girls, and their spouses outside the city limits received knowledge to make voluntary and informed choices. The initiative largely focused on complementing existing maternal and child health care programs by integrating information on different family planning methods, including long-acting reversible contraceptives (LARC) and implants, as well as non-invasive options for women and their partners.
Comprehensive Training: Equipping Providers for the Future
IHP expanded access to FP services in the supported facilities and hospitals through upskilling (teaching health workers new skills that elevate and complement their current skills) and training service providers on a range of FP services. WI-HER, through USAID IHP and in collaboration with the Hospital Management Board (HMB), PHCB, and the State Ministry of Health, organized various comprehensive training sessions focused specifically on building the capacity of healthcare workers in FP to address this increased access to FP services.
IHP deployed a holistic training approach designed to enable providers to, for example, provide couples’ counseling for family planning, offer health education targeted to men’s and boys’ health needs, appropriately serve those who desired implants, conduct difficult removals, and offer essential follow-up care to women and their spouses. This newfound expertise in family planning is crucial to ensuring the well-being of women like Martha, who seek the knowledge and benefits of FP methods.
Moreover, following the IHP healthcare worker trainings, men and women are now educated together to dispel myths and misconceptions surrounding family planning. The structured conversations moderated by healthcare professionals foster dialogue between couples to encourage shared decision-making based on informed choices while also strengthening support systems within families. Providers are prepared to meet this increased demand for FP services and are equipped with medical proficiency, empathy, and understanding to facilitate these important and life-changing conversations.
The Impact of the Family Planning Program
Following a health education session, Martha and her husband discussed what they learned about family planning, including the options that were available to them, and together they decided for Martha to receive an implant.
After the implant, Martha indicated that her life took a turn for the better since she is now in control of her reproductive choices, which she made with the support of her partner. She said, “I am happy that my husband followed me to the hospital and that we were told about family planning together… [before this health education session] no one has explained [family planning to me] as this mummy (referring to a nurse participant of LARC training) explained it today. In the next three years, I will not be pregnant again. Thank you people—my husband and I are grateful. I will tell my friends to come here and do it too.”
Jacob, Martha’s husband agreed: “I am happy that I do not have to worry about having children that I did not plan for, and I can now live happily with my wife.”
The story of Martha and her family mirrors the broader narrative unfolding across Nigeria, where informed choices and family involvement are becoming cornerstones of the healthcare journey. Through this program and targeted interventions through IHP, more men and women are discussing their family and family planning preferences together. Martha’s experience highlights the importance of family participation, and she shared her story to underscore the significance of how mutual understanding and shared decision-making within families are beneficial.
A Shared Responsibility: Paving the Way for Healthier Futures
Martha’s story, intertwined with the broader narrative of Nigeria’s healthcare transformation, illustrates the power of education and empathy. Through collaborative efforts and a shift in mindset, the nation has ushered in an era where family planning is a shared responsibility that has paved the way for healthier futures and families.
As Nigeria continues this transformative journey, amplifying the power and voices of women and the active involvement of men are not just project goals within USAID Nigeria’s IHP but are at the very heart of Nigeria’s healthcare revolution. These efforts are shaping a nation where every family can plan their future with confidence and control.
[1] Names have been changed throughout to protect the privacy of the family.